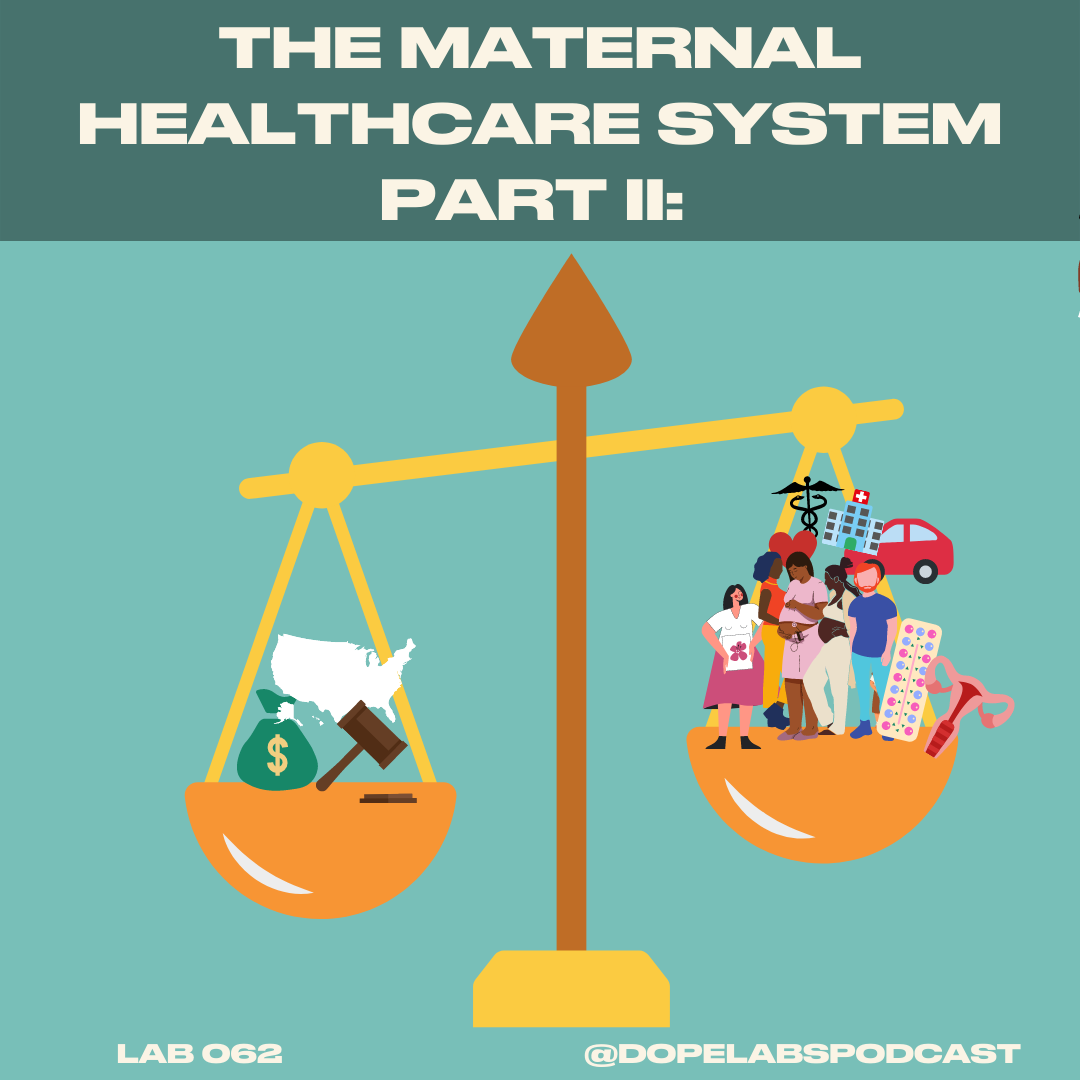
The Maternal Healthcare System Part II – Lab 063
About this Lab
The conversation around the maternal healthcare system in the U.S. is far from over, especially now when reproductive rights are further at risk. This week we continue the conversation of maternal health and we ask all the why’s. Why has the maternal mortality rate tripled in the last 40 years? Why is maternal healthcare not prioritizing mothers and birthing people after birth? Why is the maternal healthcare system failing birthing people of color? We’re getting into it all, the data, what’s changing, and what needs to change A$AP.
So many hurdles for good maternal healthcare, we darn near have to move to Finland for good services and support
Hurdles include lack of accessibility, hight mortality rates for people of color
Clearly this is not it. Why is maternal health care so bad?
No, cause something’s not making sense.
How do we make maternal healthcare work for all people?
Dr. Sarah Benatar says the U.S spends lots of money on healthcare but other high income countries have half out mortality rates
See Trends of Maternal health mortality since the early 1900s here [insert Commonwealth fund stats]
it looks at death per 100,000 pregnant people
today we’re up to 23 deaths of birthing ppl per 100,000 ppl
the mortality rate has tripled from 7 deaths per 100,000 people to 23/100000 due to discriminatory health practices and racist policy
a their of birthing people are delivering through C-section and there are more risks than birthing vaginally
mortality rates 3 to 4x higher
Black women are getting these disproportionately. WE HAVE QUESTIONS.
people who become pregnant and are then engaging in prenatal care have not necessarily had access to high quality care prior to that
Medicaid pays for over 40% of all births in the United States and for black women and birthing people, it's higher. It's more like 65% of births
Medicaid= largest payer of maternal healthcare in the U.S.
Affordable Care Act (ACA)
Why? Because before ACA, you’d typically get insurance through having a job.
In terms of pregnancy care, the medicalized model MAXIMIZES profit, creating big issues
short visits= inadequate personalized care
high no-show rates
Why?
lack of transit
maternal health deserts
lack of access to childcare
social determinants
Medicaid eligibility if different state to state and often services low income people and families
being under the federal poverty line, earning ~13k per person of ~18k for a family of 2 can absolutely affect a pregnancy
air quality
transportation
food options
state medicaid eligibility
Dr. Sarah Benatar says: Every pregnant individual in the United States who becomes pregnant should qualify for either Medicaid or the Children's Health Insurance Program
CHIP can be especially helpful for folks who may not have documentation
BUT policy like this focuses on and insures the unborn child but the parent has no access to this insurance
Postpartum care
again, birthing people are in the maternal healthcare system for 60 days after birth. NOT ENOUGH time.
the body is re-regulating and doing things like feeding the child
diapers and formula are expensive
lack of sleep for parents
this is why postpartum care is advised to continue up to 1 year after birth
Doula care can be integral to help with advocacy during the pregnancy, birthing, and after birth processes
Prenatal group care could be a viable option
The big convo around Maternal Healthcare
much more robust than in past
could use more data, data about ethnicity on medicaid claims, surveys on quality of care
mortality and morbidity is affecting Black folks who are poor and more privileged, take Serena Williams’ birthing story, for example
Congress is allocating $60 mil over next 5 years to prevent maternal mortality
medicaid that includes doula and midwifery care
Big Takeaway: the US healthcare system does not change quickly but the strides that are being made now are really transformative but should go further
#Amerie One Thing
Titi: re-dyeing clothes with Dylon.
Zakiya: Book of Addis: Cradled Embers
Guest Expert
This lab’s guest expert is Dr. Sarah Benatar, principal research associate at the Urban Institute in the Health Policy Center. She has the answers, Sway, and helps us to address a lot our why’s.
Transcript
You can read along with this lab here.